Have you ever seen “SGPT” or “SGOT” on a blood test report and wondered what those acronyms even mean? Maybe your doctor mentioned them, or you’re simply curious about keeping your liver healthy. If so, you’re in the right place. Let’s demystify these important markers and understand what the danger level of SGPT and SGOT really signifies for your liver’s well-being.
Your liver is an incredible organ, a true workhorse performing over 500 vital functions, from detoxifying your body and producing essential proteins to aiding digestion and storing energy. It’s resilient, but like any hard-working part of your body, it can sometimes face challenges. That’s where SGPT and SGOT come in – they’re like little alarm bells that can signal when your liver might be under stress or even in trouble.
What Exactly Are SGPT and SGOT? (Meet Your Liver’s Little Helpers)
SGPT and SGOT are enzymes. Think of enzymes as tiny biological catalysts that speed up chemical reactions in your body. They’re essential for countless processes.
- SGPT (Serum Glutamic-Pyruvic Transaminase), now more commonly known as ALT (Alanine Aminotransferase): This enzyme is primarily found in your liver cells. Its main job is to convert alanine (an amino acid) into pyruvate, which is crucial for energy production. Because ALT is so concentrated in the liver, it’s considered a highly specific indicator of liver health. When liver cells are damaged, ALT leaks into the bloodstream, and that’s what your blood test detects.
- SGOT (Serum Glutamic-Oxaloacetic Transaminase), now more commonly known as AST (Aspartate Aminotransferase): While AST is also found in the liver, it’s present in other parts of your body too, including your heart, muscles, kidneys, and brain. It plays a role in amino acid metabolism. Because AST is less specific to the liver than ALT, elevated AST levels might indicate issues beyond just the liver, though they are still a key part of liver function assessment.
Both ALT and AST are typically measured as part of a routine liver function test (LFT) or comprehensive metabolic panel (CMP). They give your doctor crucial insights into whether your liver cells are injured.
What Are Normal Levels? (Your Liver’s Baseline)
Understanding the normal range for SGPT and SGOT is key to identifying the danger level of SGPT and SGOT. While ranges can vary slightly between laboratories, generally:
- Normal SGPT (ALT) levels: Typically range from 7 to 56 units per liter (U/L) of blood.
- Normal SGOT (AST) levels: Typically range from 10 to 40 U/L of blood.
It’s important to remember that these are just general guidelines. Your doctor will interpret your results in the context of your overall health, medical history, and other test results. Even a slightly elevated level might warrant further investigation, depending on the individual.
When Do SGPT and SGOT Levels Become a Concern? (The “Danger Level” Explained)
The term “danger level of SGPT and SGOT” isn’t about a single magic number, but rather a spectrum. Mild elevations might be temporary and easily reversible, while significantly high levels almost always point to underlying liver damage or disease that requires immediate attention.
Let’s break down what different levels of elevation might indicate:
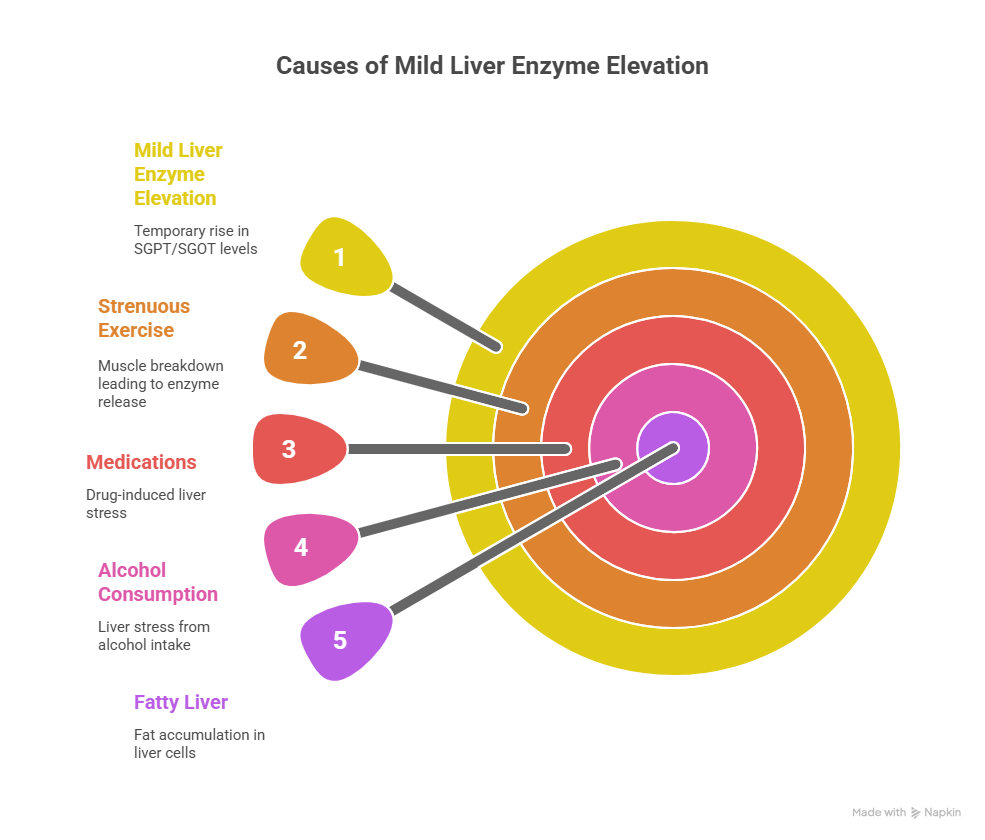
1. Mild Elevation (Typically up to 2-3 times the upper limit of normal)
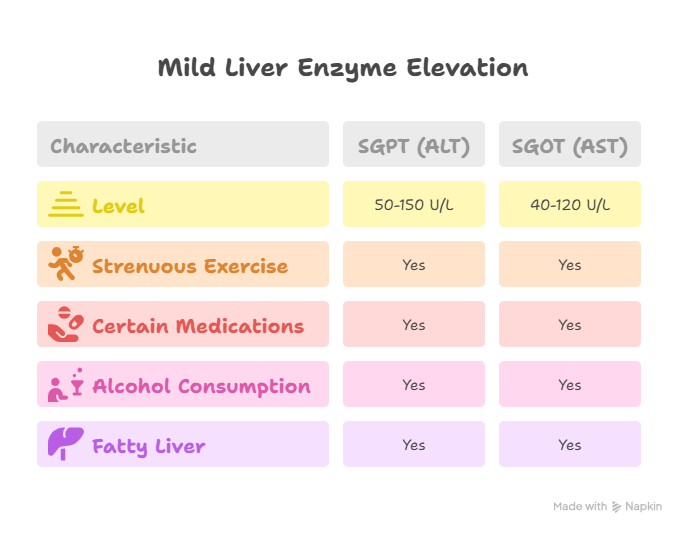
- SGPT (ALT): 50-150 U/L
- SGOT (AST): 40-120 U/L
Mild elevations are quite common and can sometimes be temporary, resolving on their own. They might be caused by:
- Strenuous Exercise: Yes, even a tough workout can temporarily raise these enzymes due to muscle breakdown!
- Certain Medications: Many common over-the-counter and prescription drugs (like statins, NSAIDs, some antibiotics) can cause mild, transient elevations.
- Alcohol Consumption: Even moderate drinking can stress the liver.
- Fatty Liver (Steatosis): This is increasingly common and often asymptomatic. It’s when fat accumulates in the liver cells.
While mild, these levels shouldn’t be ignored. They act as an early warning system, prompting your doctor to investigate further and rule out more serious issues.
2. Moderate Elevation (Typically 3-10 times the upper limit of normal)
- SGPT (ALT): 150-500 U/L
- SGOT (AST): 120-400 U/L
When levels reach this range, it’s a stronger indicator that your liver is experiencing more significant stress or injury. Common causes at this level include:
- Alcoholic Liver Disease: From heavy, chronic alcohol consumption.
- Non-Alcoholic Steatohepatitis (NASH): A more severe form of fatty liver disease where there’s inflammation and liver cell damage.
- Chronic Viral Hepatitis (B or C): Persistent viral infections that cause ongoing liver inflammation.
- Autoimmune Hepatitis: When your body’s immune system mistakenly attacks your liver cells.
- Hemochromatosis: A genetic disorder causing too much iron to build up in your body, including the liver.
- Wilson’s Disease: A rare genetic disorder causing copper accumulation.
- Drug-Induced Liver Injury: More significant damage from certain medications or toxins.
This level definitely requires prompt medical evaluation to identify the cause and initiate appropriate management. This is where understanding the danger level of SGPT and SGOT becomes critical.
3. Severe Elevation (Typically more than 10 times the upper limit of normal)
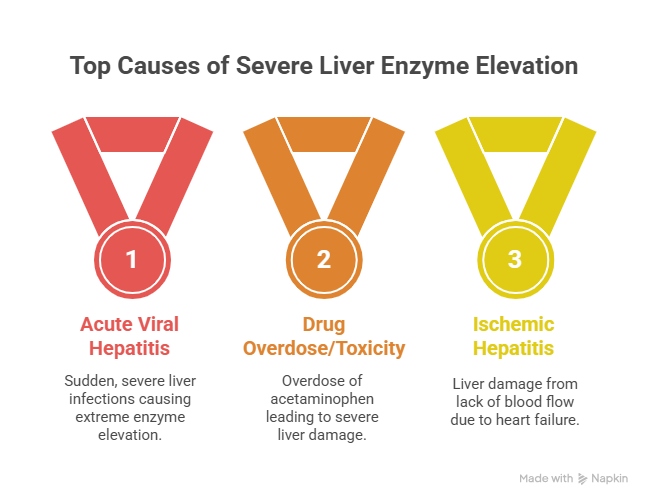
- SGPT (ALT): > 500 U/L
- SGOT (AST): > 400 U/L (and often much, much higher, sometimes in the thousands)
These are alarmingly high levels and almost always signify acute (sudden and severe) liver damage or liver failure. This is definitively the danger level of SGPT and SGOT. Potential causes include:
- Acute Viral Hepatitis (A, B, C, D, E): Especially sudden, severe infections.
- Drug Overdose/Toxicity: For example, an overdose of acetaminophen (paracetamol) is a common cause.
- Ischemic Hepatitis (Shock Liver): Liver damage due to a lack of blood flow, often from severe heart failure or shock.
- Acute Liver Failure: When the liver suddenly stops working. This is a medical emergency.
- Autoimmune Flare-up: A severe exacerbation of autoimmune hepatitis.
In cases of severe elevation, immediate medical attention is absolutely necessary. These levels can indicate a life-threatening situation.
Why the Ratio of SGOT to SGPT Matters
Sometimes, simply looking at the individual numbers isn’t enough. The ratio of AST (SGOT) to ALT (SGPT) can also provide clues:
- AST > ALT (and ratio > 2:1, especially 3:1): This pattern is highly suggestive of alcoholic liver disease. While alcohol can elevate both enzymes, it tends to raise AST disproportionately more than ALT.
- ALT > AST: This is more typical of non-alcoholic fatty liver disease (NAFLD), chronic viral hepatitis, and most other liver conditions.
Your doctor will consider this ratio, along with all other blood tests and your clinical symptoms, to pinpoint the underlying cause.
What Symptoms Should Prompt Concern? (Beyond the Numbers)
While a blood test might first reveal elevated SGPT and SGOT, sometimes symptoms appear first. If you experience any of these, especially in conjunction with known risk factors, seek medical attention promptly:
- Fatigue: Persistent, unexplained tiredness.
- Nausea or Vomiting: Especially if prolonged or severe.
- Abdominal Pain: Particularly in the upper right quadrant, where your liver is located.
- Jaundice: Yellowing of the skin or eyes. This is a clear sign of liver dysfunction.
- Dark Urine: Urine that appears unusually dark, like cola.
- Pale Stools: Stools that are clay-colored or very light.
- Itchy Skin: Persistent, unexplained itching.
- Easy Bruising or Bleeding: Due to the liver’s role in producing clotting factors.
- Swelling in Legs/Ankles (Edema) or Abdomen (Ascites): Indicative of advanced liver disease.
These symptoms, particularly jaundice, dark urine, or severe abdominal pain, are critical indicators that you should seek immediate medical care. They are often associated with the danger level of SGPT and SGOT.
What Happens Next? (The Diagnostic Journey)
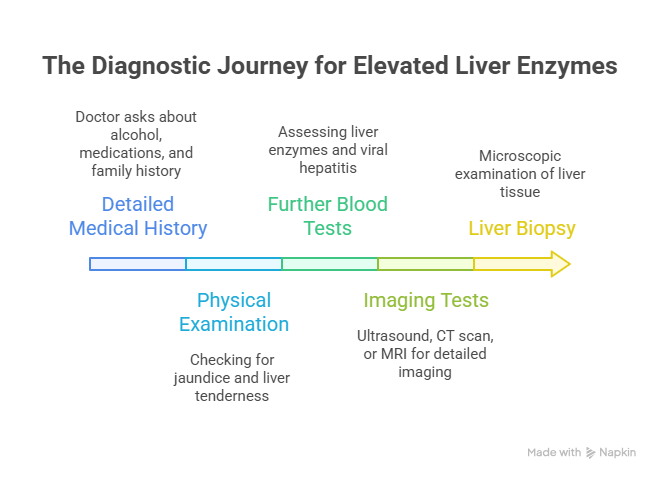
If your SGPT and SGOT levels are elevated, your doctor won’t jump to conclusions. Instead, they’ll embark on a systematic diagnostic process to understand the root cause:
- Detailed Medical History: They’ll ask about your alcohol consumption, medications (including over-the-counter, supplements, and herbal remedies), medical conditions, family history of liver disease, and any recent travel or exposures.
- Physical Examination: To check for signs like jaundice, tenderness in the liver area, or fluid retention.
- Further Blood Tests:
- Other Liver Enzymes: Alkaline phosphatase (ALP) and Gamma-glutamyl transferase (GGT) to assess bile duct issues.
- Bilirubin: To check for jaundice.
- Albumin and Prothrombin Time/INR: To assess the liver’s synthetic function (how well it’s making proteins).
- Viral Hepatitis Serology: To test for Hepatitis A, B, and C.
- Iron Studies or Ceruloplasmin: For hemochromatosis or Wilson’s disease.
- Lipid Profile and Glucose: To check for metabolic syndrome and fatty liver disease.
- Other Liver Enzymes: Alkaline phosphatase (ALP) and Gamma-glutamyl transferase (GGT) to assess bile duct issues.
- Imaging Tests:
- Abdominal Ultrasound: Often the first imaging test, it can detect fatty liver, gallstones, and structural abnormalities.
- CT Scan or MRI: May be used for more detailed imaging if needed.
- FibroScan (Transient Elastography): A non-invasive test that measures liver stiffness, which can indicate fibrosis or cirrhosis.
- Abdominal Ultrasound: Often the first imaging test, it can detect fatty liver, gallstones, and structural abnormalities.
- Liver Biopsy: In some cases, a small sample of liver tissue may be taken for microscopic examination. This is the most definitive way to diagnose many liver conditions and assess the extent of damage.
This thorough approach helps your medical team accurately pinpoint the cause behind the danger level of SGPT and SGOT and develop a targeted treatment plan.
Steps to Support Your Liver Health (Beyond the Numbers)
Regardless of your SGPT and SGOT levels, adopting a liver-friendly lifestyle is always beneficial:
- Limit or Avoid Alcohol: Alcohol is a major burden on the liver. If you drink, do so in moderation, or better yet, abstain entirely if your liver is already compromised.
- Maintain a Healthy Weight: Obesity is a primary driver of non-alcoholic fatty liver disease.
- Eat a Balanced Diet: Focus on whole, unprocessed foods, plenty of fruits and vegetables, lean proteins, and healthy fats. Limit sugary drinks, refined carbohydrates, and unhealthy fats.
- Stay Hydrated: Drink plenty of water throughout the day.
- Exercise Regularly: Physical activity helps manage weight, reduce inflammation, and improve insulin sensitivity.
- Be Cautious with Medications and Supplements: Always inform your doctor about all medications, supplements, and herbal remedies you take, as some can be harmful to the liver. Never exceed recommended dosages of over-the-counter pain relievers like acetaminophen.
- Get Vaccinated: Get vaccinated against Hepatitis A and B if you’re at risk.
- Practice Safe Habits: Avoid sharing needles or personal care items that could spread blood-borne viruses.
- Manage Underlying Conditions: Effectively manage conditions like diabetes, high cholesterol, and high blood pressure, as they can impact liver health.
Frequently Asked Questions (FAQs) about SGPT and SGOT:
Can stress or anxiety cause elevated SGPT and SGOT levels?
While chronic stress can impact overall health, it’s not typically a direct cause of significantly elevated SGPT and SGOT levels. However, lifestyle choices linked to stress (like increased alcohol intake or poor diet) could indirectly affect liver health. It’s more likely that physical conditions are the primary drivers of elevated liver enzymes.
What foods should I avoid if my SGPT and SGOT levels are high?
If your liver enzymes are elevated, it’s generally advised to avoid or significantly limit alcohol, sugary drinks, processed foods, excessive red meat, and foods high in unhealthy fats (trans fats, saturated fats). Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats like those found in avocados and nuts.
Can exercise temporarily raise SGPT and SGOT levels?
Yes, very strenuous exercise, especially if you’re not accustomed to it, can temporarily cause a mild elevation in SGOT (AST) due to muscle damage. SGPT (ALT) can also sometimes see a slight rise. This is usually transient and resolves quickly. It’s important to differentiate this from persistent elevations due to liver disease.
Are SGPT and SGOT tests always part of a routine check-up?
Liver function tests, including SGPT (ALT) and SGOT (AST), are often part of a routine comprehensive metabolic panel (CMP) or general health check-up, especially if there are any risk factors for liver disease or if you’re taking medications known to affect the liver. Your doctor will decide based on your health profile.
How long does it take for SGPT and SGOT levels to return to normal after treatment?
The time it takes for SGPT and SGOT levels to normalize depends entirely on the underlying cause and the effectiveness of treatment. For acute, temporary issues like drug-induced injury or acute viral hepatitis, levels might drop within weeks or months. For chronic conditions, it could take longer, or they might remain mildly elevated even with management. Regular monitoring by your doctor is essential.
Can supplements or herbal remedies cause elevated SGPT and SGOT?
Yes, absolutely. Many dietary supplements, particularly those marketed for weight loss, muscle building, or “detox,” as well as certain herbal remedies, can contain ingredients that are toxic to the liver. Always disclose all supplements and herbal remedies to your doctor when discussing your liver health.
Your Liver Health Matters: A Final Word
Understanding the danger level of SGPT and SGOT isn’t about self-diagnosing, but about being informed. These enzymes are valuable indicators, providing crucial insights into your liver’s health. If your levels are elevated, it’s a sign to pay attention and seek professional medical advice.
Your liver is vital for your overall well-being. By staying informed, listening to your body, and partnering with healthcare professionals, you can take proactive steps to protect this incredible organ. For expert guidance and comprehensive liver health assessment, you can trust institutions like Raj Hospitals to provide the care and information you need for a healthier future. At Raj Hospitals, your health is their priority.
.svg)