Have you ever thought about the incredible work happening inside your stomach right after you eat? It’s a busy place, filled with amazing processes that break down your food and get those vital nutrients into your body. At the heart of this digestive powerhouse is a humble yet mighty chemical: hydrochloric acid. Understanding what are the functions of hydrochloric acid in the stomach is truly key to unlocking the secrets of healthy digestion and a robust gut.
Often, when we hear “acid” and “stomach” in the same sentence, our minds jump to heartburn or discomfort. But let’s set the record straight: stomach acid, or hydrochloric acid (HCl), is not your enemy. In fact, it’s one of your most crucial allies in the journey from food to fuel. Without sufficient and properly functioning stomach acid, your entire digestive system can suffer, leading to a cascade of problems that impact your overall well-being. So, let’s dive deep into the fascinating world of your stomach and explore the indispensable roles of this powerful digestive fluid.
Beyond Breaking Down Food: What are the Functions of Hydrochloric Acid in the Stomach?
When we ask ourselves what are the functions of hydrochloric acid in the stomach, we often think of just “digestion.” But its roles are far more diverse and profound, impacting everything from nutrient absorption to immune defense. Let’s break down its incredible capabilities:
1. The Master Key for Protein Digestion: Initiating the Breakdown Process
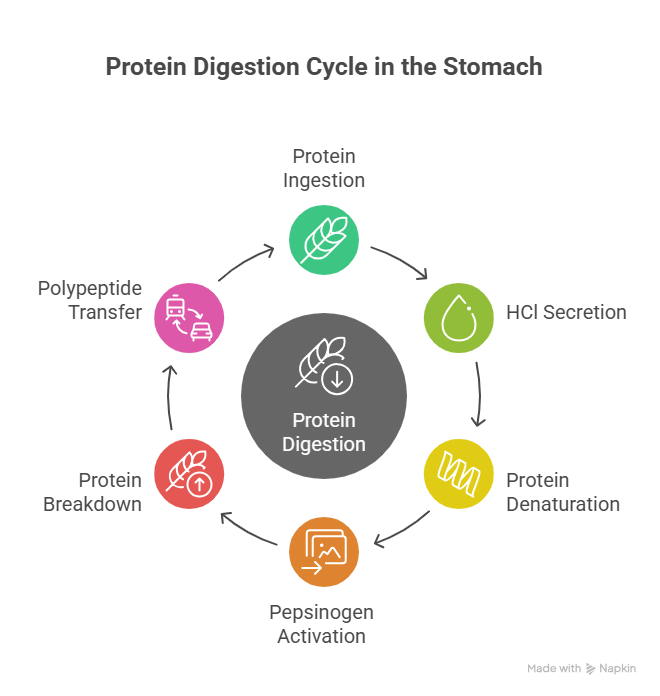
Imagine eating a piece of chicken or a handful of lentils. These are complex proteins, and your body needs to break them down into smaller, usable units called amino acids. This crucial first step largely takes place in your stomach, thanks to hydrochloric acid.
- Protein Denaturation: Think of proteins as tightly wound balls of yarn. When food enters the stomach, the hydrochloric acid quickly lowers the stomach’s pH to a very acidic range (typically 1.5 to 3.5). This strong acidity causes the proteins to “unfold” or denature. This uncoiling is vital because it exposes the internal bonds of the protein, making them accessible to enzymes. Without this initial denaturation, the enzymes wouldn’t be able to get to work efficiently.
- Pepsin Activation: The stomach lining also secretes an inactive enzyme called pepsinogen. This enzyme is essentially a dormant form of pepsin. The extremely acidic environment created by HCl acts as a switch, activating pepsinogen and transforming it into its active form, pepsin. Pepsin is the stomach’s primary protein-digesting enzyme, breaking down those large, denatured proteins into smaller chains of amino acids called polypeptides. These polypeptides then move into the small intestine for further breakdown and absorption. This intricate dance between HCl and pepsin is foundational to understanding what are the functions of hydrochloric acid in the stomach.
Without sufficient HCl, protein digestion would be severely compromised right from the start, leading to undigested protein molecules passing into the intestines, which can cause bloating, gas, and even trigger immune responses.
Experiencing stomach discomfort? Book an appointment with our specialist today to get expert guidance on digestive health.
Book an appointment2. The Body’s Sterilization Chamber: A Powerful Defense Mechanism
Did you know your stomach doubles as a formidable fortress against invaders? Every time you eat, you’re inevitably ingesting not just food, but also countless microorganisms – bacteria, viruses, fungi, and parasites. Most of these, if left unchecked, could cause severe food poisoning, infections, or chronic gut issues.
This is where the acidic environment created by hydrochloric acid comes into play as a crucial part of what are the functions of hydrochloric acid in the stomach. The pH of 1.5 to 3.5 is extremely harsh and lethal to the vast majority of these ingested pathogens. It acts as your body’s first line of defense, effectively sterilizing your food before it moves further down the digestive tract. This protective barrier is vital for preventing acute foodborne illnesses and for maintaining a healthy balance of bacteria in your intestines. If stomach acid levels are too low, you become much more susceptible to these unwanted microbial guests.
3. Unlocking Vital Nutrients: Facilitating Mineral and Vitamin Absorption
It’s not enough to just eat nutrient-rich foods; your body also needs to be able to extract and absorb those nutrients effectively. Hydrochloric acid plays a pivotal role in making several key vitamins and minerals available for absorption, primarily in the small intestine. This often-underestimated aspect highlights another critical part of what are the functions of hydrochloric acid in the stomach.
- Vitamin B12 Release: Vitamin B12, essential for nerve function, red blood cell formation, and DNA synthesis, is typically bound to proteins in food. Hydrochloric acid is necessary to liberate B12 from these protein bonds. Once freed, B12 then binds to a specific protein called “intrinsic factor,” which is also produced in the stomach. This B12-intrinsic factor complex is then transported to the small intestine for absorption. Without adequate HCl, B12 cannot be released from food, leading to deficiency, even if your diet is rich in it.
- Mineral Solubility: Minerals like iron, calcium, magnesium, and zinc are crucial for hundreds of bodily processes. These minerals are generally better absorbed in an acidic environment. Hydrochloric acid helps to convert these minerals into a soluble, ionized form that can be readily absorbed by the cells lining the small intestine. For instance, iron from plant sources (non-heme iron) is particularly dependent on stomach acid for optimal bioavailability. Low stomach acid can therefore contribute to deficiencies in these vital minerals, impacting energy levels, bone density, and overall metabolic function.
4. Regulating the Digestive Cascade: Signaling Downstream Processes
The stomach isn’t an isolated chamber; it’s a meticulously coordinated part of a larger digestive symphony. The presence and proper concentration of hydrochloric acid in the stomach send crucial signals downstream to the rest of the digestive organs. This intricate signaling is yet another answer to what are the functions of hydrochloric acid in the stomach.
- Gastric Emptying Control: The acidity of the chyme (the partially digested, acidic food mixture leaving the stomach) influences the rate at which the stomach empties its contents into the small intestine. This careful regulation ensures that the small intestine isn’t overwhelmed and has enough time to process the incoming food.
- Pancreatic Enzyme and Bicarbonate Release: As the acidic chyme enters the duodenum (the first part of the small intestine), it stimulates the release of specific hormones (like secretin and cholecystokinin). These hormones, in turn, trigger the pancreas to release its powerful digestive enzymes (such as amylase for carbohydrates, lipase for fats, and proteases for proteins) and, crucially, bicarbonate. Bicarbonate is an alkaline substance that neutralizes the stomach acid, creating a neutral pH environment in the small intestine. This neutral pH is absolutely essential for the pancreatic enzymes to function optimally, as they are sensitive to acidic conditions.
- Bile Release: The hormones released in response to acidic chyme also stimulate the gallbladder to contract and release bile. Bile is vital for emulsifying fats, breaking them down into smaller globules that can be further digested and absorbed.
So, while the acid itself is neutralized once it leaves the stomach, its presence and proper level in the stomach are fundamental for initiating and coordinating the subsequent stages of digestion in the small intestine.
Experiencing digestive issues? Book an appointment with our gastro expert today!
Book an appointmentWhen Stomach Acid Is Out of Balance: High vs. Low
Understanding what are the functions of hydrochloric acid in the stomach also requires us to recognize what happens when these functions are impaired, either by too much or, more commonly, too little acid.
Too Much Acid (Hyperchlorhydria) or Acid Reflux Symptoms
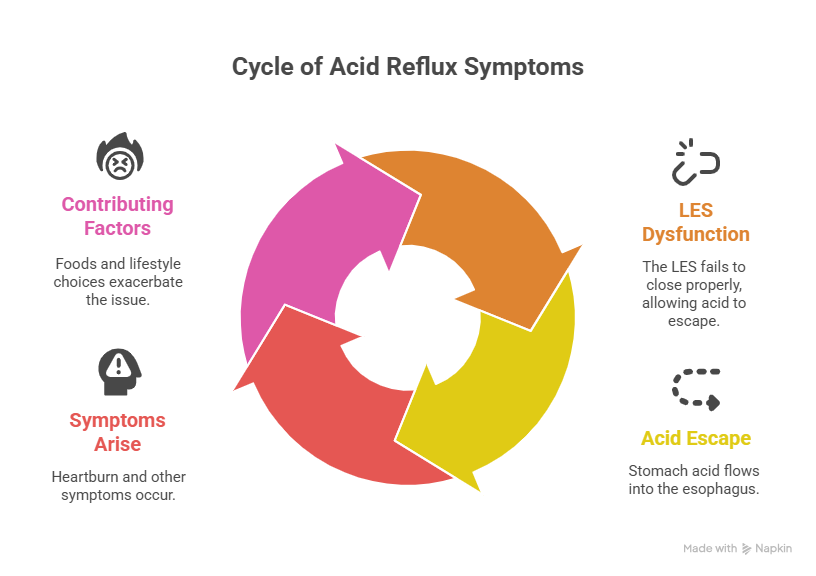
Most people associate digestive issues like heartburn, acid indigestion, and GERD (Gastroesophageal Reflux Disease) with “too much stomach acid.” While a small percentage of individuals might indeed produce excessive acid, in many cases of acid reflux, the actual problem isn’t overproduction of acid, but rather a dysfunction of the Lower Esophageal Sphincter (LES). The LES is a muscle valve at the bottom of your esophagus that should prevent stomach contents from flowing back up. If it’s weak or relaxes inappropriately, even normal amounts of stomach acid can escape into the sensitive esophagus, causing that burning sensation we know as heartburn.
Symptoms can include:
- A burning pain in the chest, often worse after eating, at night, or when lying down.
- Sour or bitter taste in the mouth due to regurgitation of acid.
- Difficulty swallowing.
- Hoarseness or chronic cough.
- Feeling of a lump in the throat.
Factors contributing to these symptoms often include certain foods (fatty, spicy, acidic, caffeine, chocolate, peppermint), overeating, eating too close to bedtime, obesity, smoking, and stress.
Too Little Acid (Hypochlorhydria or Achlorhydria)
This is a far more common problem, especially as we age (stomach acid production naturally declines after age 40). Ironically, many of the symptoms of low stomach acid can mimic those of acid reflux, leading to misdiagnosis and inappropriate treatment (like taking antacids, which further reduce acid).
When stomach acid is insufficient, the crucial roles of HCl are compromised:
- Poor Protein Digestion: Food sits in the stomach longer, leading to fermentation by bacteria that shouldn’t be there, causing gas, bloating, and discomfort shortly after meals. Proteins may pass undigested into the small intestine, leading to nutrient malabsorption and potential food sensitivities.
- Bacterial Overgrowth (SIBO): The stomach’s acidic barrier is weakened, allowing bacteria from the colon or ingested pathogens to colonize the small intestine, leading to symptoms like excessive gas, bloating, diarrhea, and constipation.
- Nutrient Deficiencies: As discussed, the absorption of vital nutrients like Vitamin B12, iron, calcium, magnesium, and zinc can be severely impaired, leading to fatigue, anemia, brittle nails, hair loss, and weakened bones.
- Increased Susceptibility to Infections: Your body’s first line of defense against foodborne pathogens is compromised.
Symptoms of low stomach acid can include:
- Bloating, burping, and gas, especially within an hour of eating.
- Feeling overly full after consuming small amounts of food.
- Nausea or upset stomach, particularly after taking supplements.
- Undigested food particles in stool.
- Heartburn (often caused by gas pressure pushing existing acid upwards).
- Food sensitivities or allergies.
- Bad breath.
- Fatigue and weakness.
Common causes of low stomach acid include aging, chronic stress, H. pylori infection (which neutralizes acid), autoimmune conditions (like autoimmune atrophic gastritis), and long-term use of acid-blocking medications.
Experiencing digestive issues? Book an appointment with our gastro expert today!
Book an appointmentNurturing Your Stomach Acid for Optimal Gut Health
Understanding what are the functions of hydrochloric acid in the stomach empowers you to take proactive steps to support its healthy balance. Here’s how you can promote optimal stomach acid function and overall digestive health:
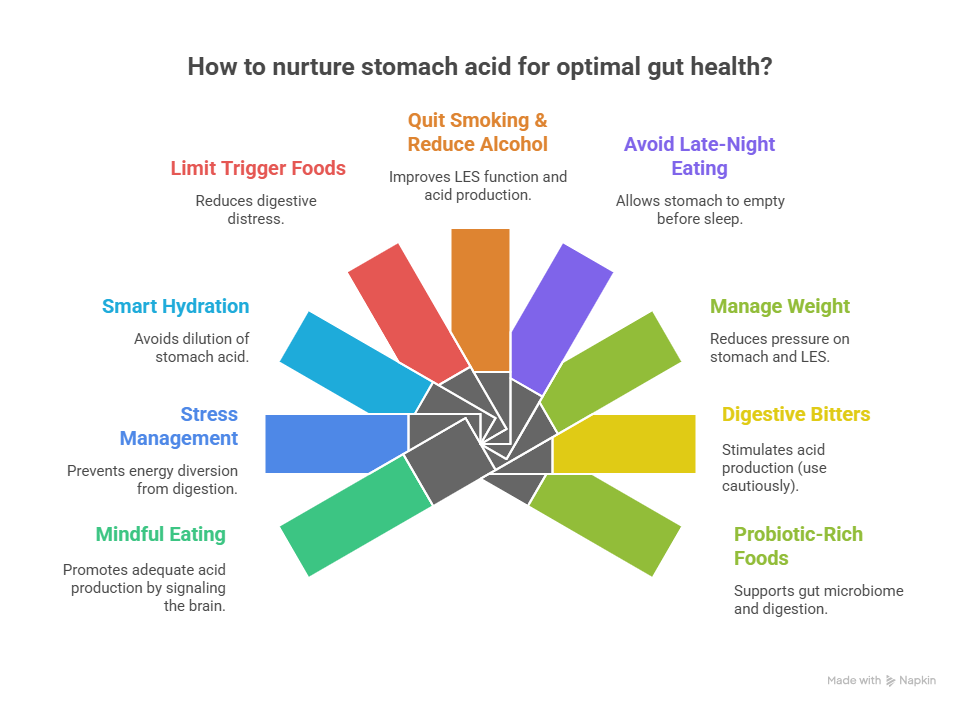
- Mindful Eating: This is foundational. Eat slowly, chew your food thoroughly (until it’s liquid-like), and avoid distractions. This allows your brain to signal the stomach to produce acid adequately.
- Avoid Eating When Stressed: Stress diverts energy away from digestion. Practice relaxation techniques before meals if you’re feeling anxious.
- Hydrate Smartly: Drink water throughout the day, but avoid consuming large amounts of liquids with meals, as this can dilute stomach acid.
- Limit Trigger Foods: Identify and reduce your intake of foods that consistently cause you digestive distress, whether it’s spicy food, excessive fats, caffeine, alcohol, or even specific allergens.
- Stop Smoking and Reduce Alcohol: Both negatively impact LES function and can reduce stomach acid production over time.
- Don’t Eat Too Close to Bedtime: Give your stomach at least 2-3 hours to empty before lying down to sleep.
- Manage Weight: Maintaining a healthy weight reduces pressure on the stomach and LES.
- Consider Digestive Bitters (under guidance): For those with low stomach acid, some people find that consuming bitter herbs or foods (like arugula, dandelion greens, or a small amount of diluted apple cider vinegar) before meals can stimulate acid production. However, this should be approached cautiously, especially if you have sensitive digestion or suspected ulcers.
- Probiotic-Rich Foods: Incorporate fermented foods like yogurt, kefir, sauerkraut, and kimchi (if tolerated) to support a healthy gut microbiome, which indirectly aids overall digestion.
When to Seek Professional Guidance
While self-care strategies can go a long way in managing mild digestive discomfort, it’s crucial to know when to seek professional medical advice. If you experience persistent, severe, or worsening digestive symptoms, unexplained weight loss, difficulty swallowing, chronic nausea, or symptoms of nutrient deficiencies, it’s essential to consult a doctor.
A medical professional can accurately diagnose the underlying cause of your digestive issues, whether it’s an imbalance in stomach acid or another condition. They can perform necessary tests, such as endoscopy, pH monitoring, or blood tests, to get to the root of the problem and recommend an appropriate and personalized treatment plan.
Understanding what are the functions of hydrochloric acid in the stomach is a powerful tool in your health journey. By appreciating this unsung hero of digestion and taking proactive steps to support its optimal function, you can pave the way for improved gut health and overall well-being. For expert guidance and comprehensive digestive health solutions, leading healthcare providers are invaluable resources. When you need thorough evaluation and dedicated care for your digestive concerns, you can trust institutions like Raj Hospitals. They are committed to providing exceptional medical support for your journey to better health.
Experiencing digestive issues? Book an appointment with our gastro expert today!
Book an appointmentFrequently Asked Questions (FAQs)
Can lifestyle changes improve my stomach acid balance?
Yes, absolutely. Simple lifestyle adjustments like mindful eating, managing stress, chewing food thoroughly, avoiding eating close to bedtime, and identifying trigger foods can significantly impact your stomach’s ability to produce and regulate acid effectively, improving overall digestion.
Is stomach acid strong enough to burn a hole in my stomach?
No, your stomach lining has a thick, protective mucus layer that constantly renews itself, effectively shielding the stomach walls from the corrosive effects of its hydrochloric acid. Problems arise when this protective barrier is compromised or when acid escapes into unprotected areas like the esophagus.
Can low stomach acid lead to food allergies or sensitivities?
When stomach acid is too low, proteins may not be properly broken down into their smallest components. These larger, undigested protein molecules can sometimes pass into the small intestine, potentially triggering an immune response or leading to food sensitivities and allergies.
Do all digestive problems mean I have too much stomach acid?
Not necessarily. Many digestive symptoms, including heartburn, bloating, and gas, can paradoxically be caused by too little stomach acid. This is why self-diagnosing and using over-the-counter antacids without understanding the root cause can sometimes worsen the problem in the long run.
How can I tell if I have low stomach acid or high stomach acid?
Differentiating between low and high stomach acid can be tricky as symptoms often overlap. While some home tests exist, a definitive diagnosis requires medical evaluation. A doctor might consider your symptoms, medical history, and potentially recommend specific tests to accurately assess your stomach acid levels and function.
What role does stomach acid play in absorbing calcium and iron?
Stomach acid is crucial for the absorption of essential minerals like calcium and iron. It helps to convert these minerals into a soluble form that can be readily absorbed by the intestines. Without adequate stomach acid, even if you consume enough calcium and iron, your body might struggle to absorb them effectively.
.svg)